THC and CBD, ingredients of cannabis, are increasingly available in various countries, particularly for medicinal use, whether available on prescription or over the counter. But their use for therapeutic purposes is still the subject of studies to determine their advantages and disadvantages, in particular for mental disorders. Here we take a look at when cannabis should be prescribed.
Cannabis: When to Prescribe It?


They are supposed to relieve gout and rheumatism, even treat malaria or constipation: they are the female flowers of cannabis, a plant of the Cannabis sativa species. As early as 2800 BCE, people in China were already using cannabis as a medicine. Later, cannabis reached India, where it was used as an antiepileptic, sedative, and anesthetic. During the Belle Époque, preparations based on this plant even enjoyed great popularity in Europe, for example as a medicine to alleviate pain. But the harsh anti-drug campaign that raged in the United States in the middle of the 20th century put a – temporary – end to the use of cannabis as “therapy”.
However, recently, thanks to ever-changing global legislation on the subject, cannabis is slowly making its way back into medicine cabinets. On the recommendation of the World Health Organization (WHO), in 2020 the United Nations Commission on Narcotic Drugs removed it from the list of the most dangerous drugs. So sooner or later cannabis will probably be marketed in many countries not only as a medicine, but also as a stimulant. This is already the case in certain American states, Uruguay, Canada, and South Africa: you can buy cannabis there in the form of cannabis – the name given to the dried female flowers – or hashish – the resin of the female plant – for personal, recreational or medical use.
This progress has all been covered in depth throughout it evolution here, and we will continue to do so. Each article is and will be available in a brief summary format, along with a link to the original in our free cannabis news app.
Cannabis is back in medicine cabinets
In France, the Ministry of Health published a decree authorizing the use of cannabis for therapeutic purposes on October 9, 2020, and an experiment was launched in March 2021 to test its effectiveness with 3,000 patients presenting with unbearable pain not reduced by conventional treatments. It is only after the analysis of the results of this trial, and some changes in French law, that doctors may prescribe cannabis in certain cases.
On the recommendation of the WHO, the United Nations Commission on Narcotic Drugs removed cannabis from the list of the most dangerous drugs in 2020. Sooner or later, cannabis will probably be marketed in many countries as a medicine or stimulant.
Elsewhere in Europe, the situation began to change a little earlier. In Germany, doctors have since 2017 the right to issue a prescription for cannabis flowers and their extracts to seriously ill patients, provided that the substances come from state-controlled crops. Another criterion for prescribing: all other therapeutic options must have been tested and proven to be ineffective.
But what would cannabis be a good remedy for? As medicines, the substances contained in cannabis are currently only recommended for a few disorders. For example, as analgesics in the case of multiple sclerosis or as anticonvulsants for severe forms of epilepsy. Given alongside chemotherapy, they are also believed to prevent nausea and vomiting that often occur during treatment. They would also stimulate the appetite of certain patients in the terminal phase of cancer or other illnesses. It is for these applications that we have been testing cannabis in France since March 2021.
Nabiximols, dronabinol, nabilone…
To do this, there are already drugs on the market composed of synthetic or natural cannabinoids and approved by certain health authorities. The latter mainly contain tetrahydrocannabinol, THC, the main psychotropic substance of cannabis, and cannabidiol, CBD, which is not psychoactive and therefore does not modify psychic functioning. For example, the drug nabiximols contains as much THC as CBD; it is used as an oral spray to relieve multiple sclerosis and chronic pain. As for dronabinol and nabilone, they are composed only of THC. And pure CBD, sold under the name “epidiolex” and already authorized in France, would reduce infantile and severe epileptic seizures. But all these drugs are sometimes taken for other disorders and, in general, in self-medication.
Cannabinoids
Cannabis sativa contains over 400 molecules, 100 of which are cannabinoids. The most important are tetrahydrocannabinol, or THC, with a strong psychotropic power, and cannabidiol, or CBD, which is non-psychoactive. These phytocannabinoids are mainly produced by the flowers of female plants. But in our body, there are also two similar molecules, called “endocannabinoids”, which bind to the same cannabinoid receptors as THC, but in a less intense way.
Indeed, people suffering from various physical or mental health problems have been using cannabis on their own for a long time. For what reasons? In 2019, an analysis of several studies based on the statements and practices of cannabis users revealed the most common reasons: pain, anxiety disorders, and depression. Some users, often “smokers” of the plant, report astonishing improvements in their mental state. But these testimonials do not in any way represent proof of the effectiveness of cannabis or of its mechanism of action. Is it simply a placebo effect – beneficial because people believe in the treatment without it having any real effect – or something more important?
Cannabis effects on mental disorders?
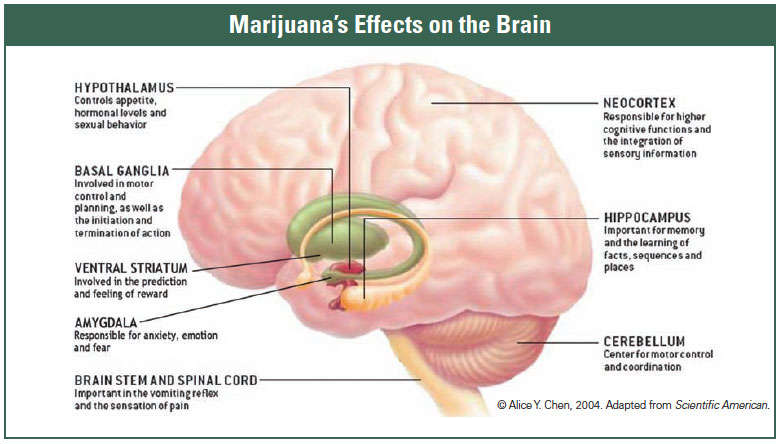
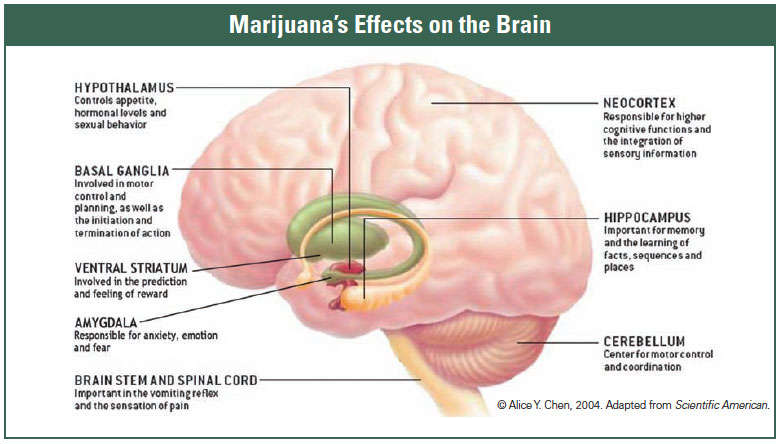
In fact, in the body and the brain, the cellular signaling pathways on which cannabinoids act, such as THC and CBD but also the “endocannabinoids” naturally present in our body, are involved in a multitude of cognitive and emotional processes. . For example, in people with schizophrenia, depression or post-traumatic stress disorder (PTSD), there are changes in the density of cannabinoid receptors in different brain regions, compared to subjects without the disorder. mental. It is therefore plausible that the consumption of cannabis influences these networks, and their cannabinoid receptors, to attenuate, or conversely aggravate, the symptoms of these pathologies.
But research on how cannabis and the endogenous cannabinoid system work is still in its infancy. Why? First, this cannabinoid system of the organism is very complex. The cannabinoid receptors involved, CB 1 and CB 2, were not identified until the 1990s, and cannabis contains hundreds of substances – not just cannabinoids – that interact with various molecules and receptors in the body and influence different signaling pathways: it is, therefore, difficult to determine which component of cannabis is responsible for which effect.
Then, because the penalization of cannabis components has hindered research, often making access to the more difficult. And industrial interest in studies with cannabis remains low because the drugs that would be derived from it do not promise a lot of money at stake. In addition, the design of the studies raises difficulties: indeed, if you want To test the effect of THC as a drug, THC in a certain form must be administered to the first group of patients, and a placebo in the same form to another group of subjects. And everyone must believe that the product they are taking contains THC, so that the effect of the molecule can be compared to that of the placebo. The problem is that you quickly realize whether the treatment you are taking contains THC or not because it has psychotropic effects. Impossible.
Cannabis is a double-edged weapon
Nevertheless, there are reasons to hope. Thanks to increasingly frequent legislative relaxations, the number of scientific publications on the subject has increased considerably in recent years. The first results suggest that cannabinoids may well alleviate the symptoms of various psychiatric disorders. But one fact is also becoming increasingly clear: cannabis is a double-edged sword! Its effect sometimes depends on the proportions of THC and CBD consumed, as well as other factors, such as the user’s age or family history.
This is shown, for example, by various studies on anxiety disorders. In theory, the cannabinoid receptors of our body represent a good pharmacological target for the treatment of mood disorders, since they are mainly present in the brain structures of the limbic system, such as the amygdala and the hippocampus, involved in the treatment of emotions. In addition, by attaching to cannabinoid receptors, THC and CBD influence the release of neurotransmitters like serotonin, norepinephrine, and glutamate, which play an important role in stress and anxiety.
Relaxation in small doses, stress in high doses
In 2019, Nicola Black and colleagues from the University of New South Wales in Sydney analyzed 84 studies on the benefits or harms of therapeutic cannabis in mental disorders. According to them, there is good evidence – although still vague – of an anxiolytic effect of THC: this substance would “relax” us. But, as is often the case in pharmacology, it is the dose that makes the potion… or the poison! Small amounts of the psychoactive cannabinoid presumably have a calming effect, while high concentrations are said to have the opposite effect, causing anxiety or even panic.
A link was confirmed in 2017 by Harriet de Wit and her colleagues at the University of Chicago. The researchers invited 42 healthy adults to take a social stress test: they had to give a speech in front of an audience. Beforehand, the volunteers consumed either tablets containing pure THC, at two different doses or a placebo composed of dextrose (having no pharmacological activity). Result: subjects who swallowed 7.5 milligrams of THC felt much less stressed during the speech than people who took the placebo. A phenomenon which, according to the researchers, would be linked to a moderating effect of THC on the activity of the amygdala. On the other hand, the individuals who took the higher dose of THC, 12.5 milligrams, were much more anxious and had more negative emotions than the others.
Similarly, CBD is a candidate for the treatment of anxiety disorders. In 2011, José Crippa’s team at the University of São Paulo gave a total of 24 people with social phobia either 600 milligrams of CBD or a placebo before having them speak out in public. Compared to the placebo, the cannabinoid had an anxiolytic effect, according to the participants’ self-assessment of their performance. In addition, the subjects who received the CBD felt in better mental shape than the others. Other work suggests that CBD also “defuses” the distressing negative effect of high doses of THC. However, it is still necessary to carry out larger and quality studies before the experts are able to formulate recommendations.
Five times higher risk of psychosis in smokers
Anyway, so far it seems that the relationship between the two substances, THC and CBD, is decisive: higher amounts of THC would be harmful, while more CBD would be rather harmless, even curative. A mechanism that appears obvious in the case of schizophrenia. Indeed, several studies show that people with a high risk of psychosis should not touch cannabis, and in the first place young people. Because the grass sometimes triggers a psychotic episode and then intensifies the pre-existing cognitive disorders. Probably because of its active psychotropic substance, THC. Although the neurobiological mechanism involved is still not well understood via CB 1 receivers. However, this dopaminergic system is also at the origin of psychotic disorders.
In 2019, Marta Di Forti, from the Royal College in London, together with British and Italian experts, conducted a study on the risk of psychosis in cannabis smokers. Researchers asked more than 900 patients who had been treated for first-episode psychosis at various clinics in Europe and Brazil about their cannabis use, then compared their responses with those of more than 1,000 healthy control subjects.
Thus, the analysis showed that people who smoke cannabis with a THC content of more than 10% every day are approximately five times more likely to have a psychotic episode. According to the researchers, the number of schizophrenics in Amsterdam, where very strong weed consumption is common, would be halved if the daily use of cannabis were banned. Other scientific studies also confirm that cannabis increases the risk of psychosis.
CBD, an antipsychotic?
On the other hand, CBD, meanwhile, is attracting the attention and interest of scientists because, unlike THC, it is said to have antipsychotic power. Indeed, in 2011, the team led by Christian Schubart, from the University Medical Center in Utrecht, conducted an online survey of approximately 2,000 cannabis users. Frequency and types of consumption were collected, as well as any psychotic symptoms, using a standardized questionnaire. The researchers were able to carry out this study because cannabis is a legal stimulant in the Netherlands under certain conditions: they, therefore, had access to the THC and CBD contents of the various products consumed.
Result: the more cannabis contains CBD, the less risk smokers have of having a psychotic episode, regardless of the THC content. But other studies have not found this effect, probably because the age of the consumers again plays a role: one theory suggests that CBD would only be suitable as a complementary therapy in the early stages of schizophrenia. Many questions, therefore, remain open. However, Eva Hoch, a psychologist and cannabis researcher at the Ludwig-Maximilian University Clinic, Munich, believes there is still value in further investigating the antipsychotic potential of CBD.
Cannabis and mood improvements
Another contemplated benefit of cannabis: many people claim to smoke or use cannabis because of its positive effects on mood. Could cannabis help fight the symptoms of depression? This question remains hotly debated from a scientific point of view. But one study found that depressed women have reduced levels of endocannabinoids in their brains, compared to mentally healthy people. And the lower the concentration of endocannabinoids in the brain, the longer the bad mood lasts, according to another study by Matthew Hill’s team at the University of British Columbia in Vancouver, published in 2008.
What’s more, cannabinoids influence the release of neurotransmitters, especially in the limbic system, and therefore sometimes have a relaxing and euphoric effect. A further clue to their benefit on mood. But despite these results and the many positive reports from consumers, the therapeutic potential of cannabis on depression has not been studied so far: clinical studies on the subject are sorely lacking.
However, a handful of observational studies and feedback do suggest an antidepressant effect. Staci Gruber, of McLean Hospital, Belmont, found that smoking cannabis somewhat alleviated the depressive phase of subjects with bipolar disorder. But, again, there are sometimes paradoxical effects: moderate cannabis consumption seems to improve the mood of these patients in the short term, but excessive consumption has the opposite effect and even intensifies their depressive symptoms.
Recover from trauma?
For some time, it has also been known that many people with post-traumatic stress disorder (PTSD), for example, victims of an attack, often smoke cannabis, presumably to self-medicate. In Canada and the United States, medicinal cannabis is already approved as a treatment for trauma. This suggests some harmlessness. But, here too, caution is in order.
Indeed, some studies on THC and CBD highlight a possible therapeutic benefit. For example, in several studies, nabilone, containing only THC, improved the sleep of trauma patients, in particular by reducing their nightmares. Experiments with animals have also shown that the amygdala, involved in the control of emotions, in particular fear, is highly dependent on the endogenous cannabinoid system: the saturation of its cannabinoid receptors by active molecules of cannabis could modify its functioning and promote the forgetting of unpleasant, frightening memories.
However, in 2020, Sabrina Botsford, from the University of Toronto, came to the opposite conclusion: cannabis would increase the symptoms of PTSD instead of alleviating them. The American Academies of Sciences, Engineering, and Medicine (NASEM) therefore believe that the scientific studies carried out to date are insufficient to rule on the therapeutic effect of cannabis in the case of post-traumatic stress disorder.
It’s a whole different story when it comes to chronic pain, those that last several months, sometimes without apparent cause! According to Nasem, scientific evidence already points to a benefit of cannabis. Today, pain is by far the main reason for prescribing medicinal cannabis: 70% of cannabis prescriptions made in the world mention this indication. Especially since almost one in five of the planet’s inhabitants suffer from persistent pain. In addition to medication, doctors also use physical exercise and psychological therapies to treat chronic pain. But often that is not enough.
Effective pain relief with cannabis
However, the endogenous cannabinoid system is best known for its role in pain control, through its interaction with the pain circuit. However, only a few studies clearly show the positive effects of cannabis or its components on nociceptive signaling pathways. So currently treatment with cannabis is only recommended in the case of neuropathic pain, that caused by damage to the nerves.
Indeed, recently, a new scientific analysis, carried out by Michael Überall, vice-president of the German Society for Pain Medicine (DGS), concluded that the drug nabiximols (comprising THC and CBD) effectively complements other treatments. for pain, like morphine. Both cannabinoids are thought to amplify the pain-relieving effects of other therapies. On the other hand, Überall considers that the use of nabiximols for other reasons, such as acute or cancer-related pain, would be less appropriate… But adding, despite everything, that the anxiolytic and relaxing effect of cannabinoids would facilitate the management of long-term pain of any kind.
In several studies, nabilone, containing only THC, improved the sleep of trauma patients, in particular by reducing their nightmares.
Today, another major question regarding medical cannabis remains unanswered: do cannabinoids interact with other drugs and, if so, how? Dosage, route of administration, age and gender of the patient would play an unexpected role in efficacy. In addition, many people consume cannabis in the form of a joint, often mixed with tobacco. However, it is clearly established that smoking is dangerous for health and, in fact, smoking cannabis would cancel all its positive effects and would therefore be harmful.
Room for more cannabis research
In 2018, a research group led by Fiona Clement of the University of Calgary Cummings School of Medicine published a review of the literature on the main risks of smoking cannabis: increased risk of cerebrovascular accident and cancer of the testicles, impairment of memory and learning, structural modifications of the brain. In addition, there are dysfunctions of various cognitive functions, such as attention, as well as psychological disorders, including psychoses, manic disorders, and an increase in the number of suicides. Factors to be taken into account according to each patient when considering the use of cannabis in therapy, insist the researchers.
Eva Hoch, however, would like to see more evidence-based recommendations. Physicians should therefore always carefully consider the effects to be expected in each patient, as well as the risks and contraindications. The German Society for Pain Medicine recommends prescribing ready-to-use drugs with clearly defined levels of THC and CBD rather than cannabis in flower form, because the former are better studied, less risky, and easier to dose than the female flowers themselves.
It will therefore be understood: many questions still remain unanswered. But the legalization of cannabis is evolving almost everywhere in the world and is stimulating research on its beneficial and harmful effects. Germany and France are still far behind in this area. But, slowly, things are changing: in 2019, the German government set up a network to promote research on cannabis and the cultivation of the plant in Germany, and, after the French experimentation on therapeutic cannabis, it is likely to be prescribed by prescription for some patients. So it remains to be seen whether the future of medicinal cannabis will be bright or nebulous.
__
(Featured image by Esteban Lopez via Unsplash)
DISCLAIMER: This article was written by a third-party contributor and does not reflect the opinion of Hemp.im, its management, staff, or its associates. Please review our disclaimer for more information.
This article may include forward-looking statements. These forward-looking statements generally are identified by the words “believe,” “project,” “estimate,” “become,” “plan,” “will,” and similar expressions. These forward-looking statements involve known and unknown risks as well as uncertainties, including those discussed in the following cautionary statements and elsewhere in this article and on this site. Although the Company may believe that its expectations are based on reasonable assumptions, the actual results that the Company may achieve may differ materially from any forward-looking statements, which reflect the opinions of the management of the Company only as of the date hereof. Additionally, please make sure to read these important disclosures.
First published in Pour la Science, a third-party contributor translated and adapted the article from the original. In case of discrepancy, the original will prevail.
Although we made reasonable efforts to provide accurate translations, some parts may be incorrect. Hemp.im assumes no responsibility for errors, omissions, or ambiguities in the translations provided on this website. Any person or entity relying on translated content does so at their own risk. Hemp.im is not responsible for losses caused by such reliance on the accuracy or reliability of translated information. If you wish to report an error or inaccuracy in the translation, we encourage you to contact us.



Comments are closed for this post.